Healthcare
Diabetes with Continous Glucose monitoring
CGM devices changing the dynamics of diabetes
Diabetes is a chronic condition that affects millions of people worldwide. It occurs when the body either does not produce enough insulin or cannot properly use the insulin it does produce. Insulin is a hormone that regulates blood sugar levels, so when insulin production or usage is impaired, blood sugar levels can become too high or too low, which can lead to a wide range of health complications.
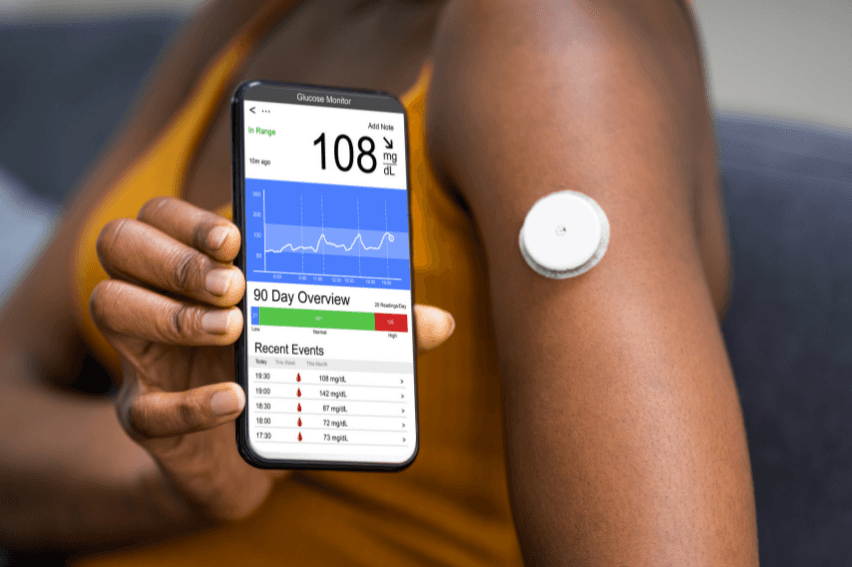
One of the key tools for managing diabetes is continuous glucose monitoring (CGM). CGM involves wearing a small sensor on your skin that measures your blood sugar levels every few minutes and sends the data to a receiver or smartphone app.

This allows people with diabetes to track their blood sugar levels in real-time and make informed decisions about their diet, exercise, and insulin dosing.
Benefits of CGM
There are several benefits to using CGM for diabetes management:
Improved blood sugar control: CGM provides continuous data about blood sugar levels, allowing people with diabetes to make more informed decisions about their diet, exercise, and insulin dosing. This can lead to better blood sugar control and fewer complications from diabetes.
Increased awareness: CGM can help people with diabetes become more aware of how their daily habits affect their blood sugar levels. For example, they may notice that their blood sugar levels are higher after eating certain foods or that they need more insulin after exercising.
Early detection of problems: CGM can alert people with diabetes to potential problems before they become serious. For example, if blood sugar levels start to drop too low, the CGM device can sound an alarm, prompting the person to take action to raise their blood sugar levels.
Reduced stress: CGM can help reduce the stress and anxiety that often comes with managing diabetes. Instead of constantly worrying about blood sugar levels, people with diabetes can check their CGM device to see how they are doing.
Improved quality of life: By providing continuous data about blood sugar levels, CGM can help people with diabetes feel more in control of their condition. This can lead to a better quality of life and a greater sense of well-being.

There are several different types of CGM devices available, each with their own pros and cons. Some devices require a prescription from a healthcare provider, while others are available over-the-counter. It is important to work with a healthcare provider to determine which device is right for you. In conclusion, continuous glucose monitoring is an important tool for managing diabetes.
By providing continuous data about blood sugar levels, CGM can help people with diabetes make informed decisions about their diet, exercise, and insulin dosing, leading to better blood sugar control and a better quality of life. If you have diabetes, talk to your healthcare provider about whether CGM is right for you.
Future of CGM
Continuous glucose monitoring (CGM) technology has already made a significant impact on diabetes management by providing real-time, accurate information about glucose levels. However, there is still room for improvement and innovation in the future of CGM.
Here are some potential developments that could shape the future of CGM:
Improved accuracy: Despite significant advancements, current CGM devices still have limitations in accuracy, especially during rapid changes in glucose levels or in the presence of certain medications or substances. Researchers are exploring various strategies to improve accuracy, such as developing better sensor algorithms or incorporating multiple sensors for redundancy.
Integration with closed-loop systems: CGM technology is a key component of closed-loop or artificial pancreas systems, which automatically adjust insulin delivery based on glucose readings. In the future, CGM technology could be further integrated with closed-loop systems to improve overall glycemic control and reduce the burden of diabetes self-management.
Non-invasive or minimally invasive sensors: Current CGM devices require insertion of a small sensor under the skin, which can be uncomfortable and may cause skin irritation. Researchers are working on developing non-invasive or minimally invasive sensors that can measure glucose levels without skin penetration, such as optical or sweat-based sensors.
Personalized medicine: CGM data can provide valuable insights into individual glucose patterns and trends, which can inform personalized treatment plans. In the future, CGM technology could be further personalized to individual needs and preferences, such as by integrating with other health data or using artificial intelligence algorithms to optimize treatment recommendations.



